It is common practice to maintain a temperature of 37 oC during all working and culture conditions in the IVF laboratory. This will allow for an optimal environment for the handling and culture of gametes and embryos. In this blog post I will explain why temperature control in the IVF lab is crucial, what equipment to be measured, when to measure and what to do with the results.
Keeping control of temperature is crucial for successful treatment
During the early stages of embryo development, major epigenetic reprogramming takes place that is crucial for the normal fate of the embryo. Changes in environmental conditions, including temperature, can affect the stability of the epigenetic reprogramming process1. When temperatures drop or rise too far away from 37 oC, it can lead to detrimental and irreversible damage in some cases to the gametes and embryos. Thus, it is of utmost importance to maintain this constant temperature during all events that take place in the IVF laboratory when a patient is undergoing treatment. Equally important is the temperature at which we store our culture media – deviations from the correct storage temperature for prolonged periods could affect the quality of the culture media and this also the development of the gametes and embryos.
What equipment do we measure and why?
All laboratory equipment that are either in direct or indirect contact with gametes and embryos or the culture media, must be carefully monitored in an accurate way. The following are examples of the most common and important pieces of equipment that we have to control the temperature of:
- Incubators
- Heated stages
- Warming blocks/ovens
- Refrigerators/Freezers
- Ambient temperature
The gametes and embryos spend the longest part of their journey through the IVF lab inside the incubators and it goes without saying that these pieces of equipment should be really well monitored, and nontheless so the temperature. You should never only rely on the temperature display of your incubator for an accurate reading. Make use of another independent thermometer or probe to verify the temperature display on the incubator.
Whenever we work with gametes and embryos outside of the incubators we rely on heated stages to maintain the temperature of 37 oC inside the dishes. Only when you use dishes that are specifically designed, made and tested for IVF by a reputable supplier will the temperature inside the media of the dish be at 37 oC when the stage is set at the same temperature. In all other dishes that are routinely used in the IVF lab, the temperature inside the dish will be well below 37 oC when the stage is set at 37 oC. This is due to the fact that there is an air gap of various distances, depending on the dish, between the bottom of the dish and the heated stage. Be sure to validate and calibrate your heated stages correctly to maintain a temperature of 37 oC in the media inside the dish and not just 37 oC on the heated stage.
The use of warming block/ovens is also common in the IVF lab to maintain the temperature of culture media and follicular fluid for instance during procedures. When you are making use of heating blocks especially, make sure not to fill tubes with media above the height of the block itself – it will otherwise expose some part of the media inside the tube that is not heated by the block and thus a variation or gradient in temperature may occur. Again, make sure to measure the temperature inside the media contained in the tube and not the heated block itself.
It is also common that we measure and control the ambient temperature in the laboratory as well as the oocyte collection theatre and embryo transfer room. Seasonal changes could have an effect on the culture media temperature inside the dishes, even if the heated stages remained set at the same temperature. This is due to the drop or rise in ambient temperature. One must not forget that there may be a prolonged exposure to temperature during the oocyte collection and embryo transfer procedures when the oocytes are either passing through the tubing of the oocyte collection needle or held in the collection tubes with the follicle aspiration fluid. After loading an embryo inside an embryo transfer catheter, the temperature may also drop very rapidly when the ambient temperature is too low or when there is additional airflow due to an air conditioner that may cool down the catheter.
The control of the temperature of refrigerators and freezers where we keep our culture media is extremely important. We spend a lot of effort on monitoring the temperatures of heated stages and incubators, and we should do this with the equipment that stores our very important and sensitive culture media as well. Once a culture media manufacturer has dispatched the shipment of media and can provide proof of validation that the temperature is well regulated during transport, it becomes the responsibility of the laboratory on arrival. Make sure the culture media is transferred and stored immediately upon arrival in a certified medical grade refrigerator that will be able to create a homogeneous temperature throughout the chamber during storage. It is also extremely important to follow the manufacturer’s recommended storage conditions.
Use a measuring device suitable for what you are measuring
There exist several different temperature measuring devices on the market today, from electronic thermometers with thermocouples to data-loggers, temp-tracers and continuous temperature monitoring probes that can be connected to a clinic’s IT network and the internet for instant access and easy monitoring and adjustment.
There is no single measuring device which is the best to use. But it is important is to use a measuring device that is suitable for the type of equipment that needs to be monitored. If you need to measure the temperature inside a culture media micro droplet, then it is obvious that you will need a very fine thermocouple connected to an electronic thermometer and you cannot use a data-logger or “thermo-coin”.
Be sure to understand how to use the equipment properly while doing a measurement and that it is serviced, by a certified service engineer or qualified technician, on a regular basis. This will prevent inaccurate readings or drifts in deviations from the measured value. These measuring devices are not meant to last forever and will need to be replaced after some time. The frequency of use and the way that you work with and look after the equipment will play a huge role in its life expectancy. It is often only necessary to replace certain parts of the devices. For instance, an electronic thermometer can last a long time and it would only be necessary to change the thermocouples from time to time.
Consistency in measurements is the key
Consistency is the most important thing to remember when it comes to doing measurements with a thermometer. We have protocols in place for every procedure that we perform during the IVF process, and so too should we have protocols in place for measuring temperature. When using automated continuous temperature monitoring systems, we are able to reduce the number of variables during the measuring procedure. The same is not true when we are using a handheld device. Therefore, make sure that every measurement for a specific piece of equipment and process is always repeated in exactly the same way.
It is good practice to check from time to time that everybody responsible for these measurements, do it in exactly the same way and follow the protocol. For instance, Figure 1 below indicates measurement of temperature in a micro droplet of a culture dish taken from the incubator and placed on a heated stage. If the total length of the thermocouple, exposed to warm culture media and oil cover, is more in one measurement than the other, you will end up getting different readings. The distance of the fingers from the measuring tip may also affect the reading due to the temperature of the fingers that are carried over to the thermocouple.
The frequency of measurements is also dependent on the equipment and specific procedure. Make use of your own validation and tested protocols to establish how often a certain measurement needs to be taken.
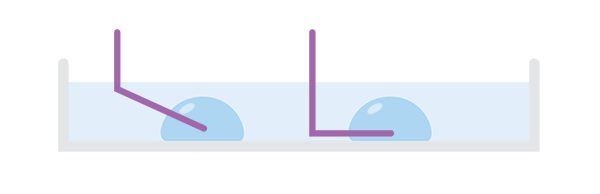
Figure 1: Temperature measurement in micro droplets under oil with 2 different lengths of the thermocouple exposed to warm media and oil.
When measuring the temperature of incubators, be sure to do that first thing in the morning before the doors are opened. As soon as the incubator doors are opened with the start of the work day, the internal temperature is disturbed and may take a while to recover. In humidified incubators, the % water vapour in the air will also have an effect on the temperature and will change once the doors have been opened.
It is common in some laboratories to do temperature mapping inside incubators and refrigerators as well as on heated stages to identify any cold or hot spots. In most good quality equipment these so called temperature spots are much reduced but it is still valuable to do this exercise to be sure. When these temperature spots are identified, try to avoid them where possible during the IVF procedures. The best option will be to make use of equipment with a homogeneous temperature distribution.
If you are going to measure the temperature in a specific dish for a specific procedure, make sure that the dish set up is exactly the way it would be during your normal work procedure. In other words, when a procedure is performed with the lid of the dish removed (ICSI for instance), then you have to do the measurement with the lid removed as well. When an air filtration system is switched on during the procedure, then make sure it is also switched on when the measurement is done. Set up each measuring exercise to mimic each IVF process, dish and equipment exactly. The time over which the measurement is taken should also reflect the same time that the dish and media will be exposed to the external environment.
Unless you are using dishes that are specifically made, designed and tested for IVF, you cannot assume that the temperature in one dish will be the same in a different dish during the same procedure. Make use of a trusted and reputable manufacturer and supplier of your disposable devices – after all, the gametes and embryos will be placed here for up to a number of days during the IVF process.
Use your results to work for you
Recordkeeping goes hand in hand with monitoring and it is extremely important to make sure we use the results that we obtain. Each laboratory is unique and will display certain characteristics that will determine how changes made in the laboratory will affect the outcome. If we notice that a piece of equipment is consistently out of range during a certain time of day, it could be related to secondary actions taking place at that time that affects the equipment. If variables like these can be eliminated and the equipment is still consistently out of range we need to consider calibration, servicing or even replacement.
Reviewing our temperature measurements and comparing it to our outcomes over longer periods of time may also reveal certain truths. We may find that seasonal temperature changes may affect the ambient temperature in our laboratories which can then have an impact on the performance of certain pieces of equipment. For instance, high ambient temperatures are not suitable for the optimal operation of incubators. It has been reported that during very warm summer months, the incubators will go into alarm more often because of the inability of certain incubators to function properly if the ambient temperature is within 10 oC of its set operating temperature.
Review and interpret the measured results - it will allow you to make changes in your IVF procedures that could improve the embryo development and ultimately the outcomes of the laboratory. Use temperature measurements as a tool to work for you.
Want to learn more?
Watch a presentation by Jaco Geyer on the topic "The value of quality control and quality assurance - it´s in the details".
References:
- Ventura-Junca, P. et al. In vitro fertilization (IVF) in mammals: epigenetic and developmental alterations. Scientific and bioethical implications for IVF in humans. Biol Res. 2015 Dec 18;48:68. doi: 10.1186/s40659-015-0059-y
Topics: IVF laboratory control, Embryo culture & transfer
Written by Jaco Terblanche
When there is a problem in a clinic needed to be solved, Jaco is never far away. This former Lab Manager now spends his working time travelling around the globe to support IVF clinics to improve their results.
