The concept of fast freezing or vitrification was first described more than 80 years ago by Basile J. Luyet, the so-called Father of Cryobiology (Luyet, 1937). He showed that supercooled solutions could be solidified without crystallization, forming a glass-like state. Already then, the potential of the technique and the associated challenges were in the research spotlight. Today, we’ve managed to overcome all methodological-related issues of vitrification. It has evolved into a reliable and efficient method to freeze oocytes and embryos. Vitrification is used for medically assisted reproduction and fertility preservation: the goal is to ensure the maximum survival rate with the highest level of biosafety. In this blog post, we will compare closed and open carrier devices for vitrification.
Why are there two types of vitrification devices?
The main principle of vitrification, to avoid ice crystal formation during cooling, storage and warming, can be equally achieved using a closed or open vitrification device. The key difference is that open devices expose the sample directly to the environment, whereas closed devices protect the sample from potential disease transmission from the environment. The invention of closed devices followed medical requirements for aseptic handling of oocytes and embryos during the entire in vitro fertilization (IVF) procedure.
Liquid nitrogen-mediated transmission of infectious agents was proven under experimental conditions
 Sources of contamination during cryopreservation include exposure to non-sterile liquid nitrogen, cross-contamination of pathogens between samples during storage, unsterilized storage tools (canisters, holders) and using dewars that have not been decontaminated. To avoid these risks, biological samples can be successfully vitrified inside sterile straw and then hermetically sealed using the closed Rapid-i vitrification system, which prevents direct contact between oocyte/embryo and liquid nitrogen.
Sources of contamination during cryopreservation include exposure to non-sterile liquid nitrogen, cross-contamination of pathogens between samples during storage, unsterilized storage tools (canisters, holders) and using dewars that have not been decontaminated. To avoid these risks, biological samples can be successfully vitrified inside sterile straw and then hermetically sealed using the closed Rapid-i vitrification system, which prevents direct contact between oocyte/embryo and liquid nitrogen.
Health authorities around the globe are cautious about possible contamination when using open vitrification devices.
Liquid nitrogen-mediated transmission of infectious agents is not just a theory, but a proven reality under experimental conditions (Bielanski et al., 2000; Bielanski et al., 2003; Bielanski and Vajta, 2009). Furthermore, several cases of hepatitis B virus transmission to patients were reported due to cross-contamination of biological samples stored in liquid nitrogen (Tedder et al., 1995). Considering all the possible contamination sources for vitrified samples, it is surprising that no IVF-related case has been reported (Vajta et al., 2015). But could contamination of vitrified/warmed oocytes/embryos explain why some frozen embryo transfers fail to implant? The use of the closed device eliminates the potential contamination of oocytes/embryos during vitrification and storage. Indeed, global health authorities are cautious about possible cross-contamination during storage or handling when using open vitrification devices (De Munck et al, 2016).
An experimental study using the Cryotop open device demonstrated that 45 % of samples became contaminated after just 10 seconds of contact with contaminated liquid nitrogen (Criado et al., 2011). In the same study, no samples were contaminated when a closed device was used. In the light of the COVID-19 pandemic, it is imperative to follow the highest biosafety protocols and use closed vitrification devices (ESHRE 2020; Adiga et al., 2020).
Using a closed device guarantees 100 % protection from possible contamination.
Some medical centers do not consider liquid nitrogen-mediated contamination to be a risk for frozen biomaterial. Yet, all clinics store gametes and embryos from patients who are hepatitis/HIV positive in a separate dewar to avoid cross-contamination between positive and negative patients. Is “low” an acceptable risk for our patients? Using a closed device guarantees 100 % protection from possible contamination.
Cooling and warming rates
Cooling rates were a key focus for embryologists for many years, as vitrification requires a sufficiently high cooling speed. Carrier devices have evolved from simple electron microscopy grids to a vast array of commercially available carriers including open pulled straws (Vajta et al., 1998), Cryoloop (Lane et al., 1999), Cryotop (Katayama et al., 2003) and Cryolock (Bernal DP et al., 2009). These are open vitrification devices, which provide very high cooling speeds. However, it has long been recognized that even if vitrification is successful, the sample can still be damaged by ice crystal formation during warming (Luyet and Gehenio, 1940). Considering cooling speed only does not guarantee the best success rates.
Rapid-i Kit combines a sufficiently high cooling speed with a very high warming speed
An experimental study on mouse oocytes demonstrated that a relatively moderate cooling rate of 522 °C/min was sufficient to ensure high survival rate if it was followed by a very high warming rate of 2950 °C/min (Seki and Mazur, 2009). Knowledge of this phenomenon paved the way for the successful clinical use of the closed vitrification device, Rapid-i Kit, which prevents direct contact between the sample and liquid nitrogen and combines a sufficiently high cooling speed with a very high warming speed. Clinical studies comparing vitrification with closed (Rapid-i Kit) and open devices (Cryotop) demonstrated that the survival rates were better for human oocytes (Pujol et al., 2019) and similar for blastocysts (Hashimoto et al., 2013).
Rapid-i Kit as the gold standard of efficient and safe vitrification

The oocyte survival rate was found to be higher using the Rapid-i Kit than the Cryotop device.
Pujol et al., 2019
The cooling rate depends on the shape and volume of the drop of vitrification media containing the sample. Incorrect loading of an open device may reduce the cooling rate if the drop is too big or cause mechanical damage to the sample if the drop’s shape is wrong. 
These problems are not an issue with the Rapid-i Kit. The Rapid-i stick has a pre-defined aperture, which is easy to fill with the correct volume of vitrification media. Oocytes or embryos are held on the Rapid-i stick by surface tension and do not contact the device itself. Thus, the issue of shape doesn’t exist: the sample is suspended in a thin film of vitrification solution. Using the Rapid-i Kit is the best way to standardize the loading process and reduce variability between operators. Another advantage of the Rapid-i Kit is that it functions as a closed device for cryopreservation, but as an open device for warming. The Rapid-i stick with the sample is directly immersed into warming media ensuring the highest possible warming rate.
Loading with Rapid-i Kit is standardized thanks a pre-defined aperture, which is easy to fill with the correct volume of vitrification media.
The comparison between Rapid-i Kit vs Cryotop

A recent study comparing the Rapid-i Kit with the Cryotop for vitrification/warming of human donor oocytes, demonstrated that the survival rate was significantly higher with the closed system (Pujol et al., 2019). Results from multiple studies using the Rapid-i Kit show excellent survival and clinical pregnancy rates for oocytes, cleavage stage embryos and blastocysts.
Table 3. Oocyte and embryo survival rates using closed devise Rapid-i Kit and open device Cryotop (Pujol et al., 2019).
| Rapid-i Kit (Closed) | Cryotop (Open) | |
| Number of vitrified and warmed oocytes | 498 | 474 |
| Survival rate, % | 94.6* | 88.8 |
| Number of vitrified cleavage-stage embryos | 25 | 16 |
| Survival, % | 100 | 100 |
*p<0.01 vs Cryoptop
Clinical outcomes after vitrification using the Rapid-i Kit
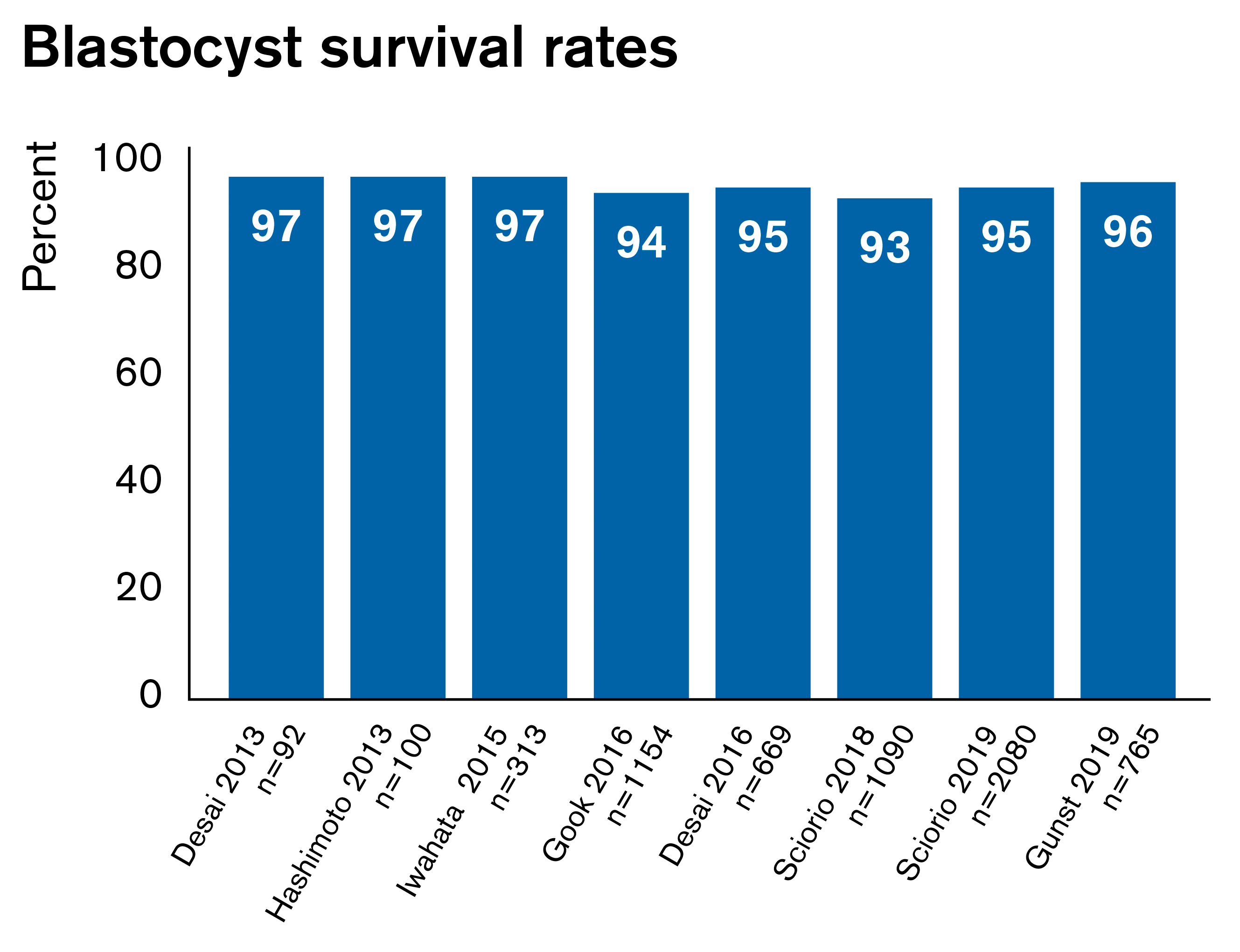
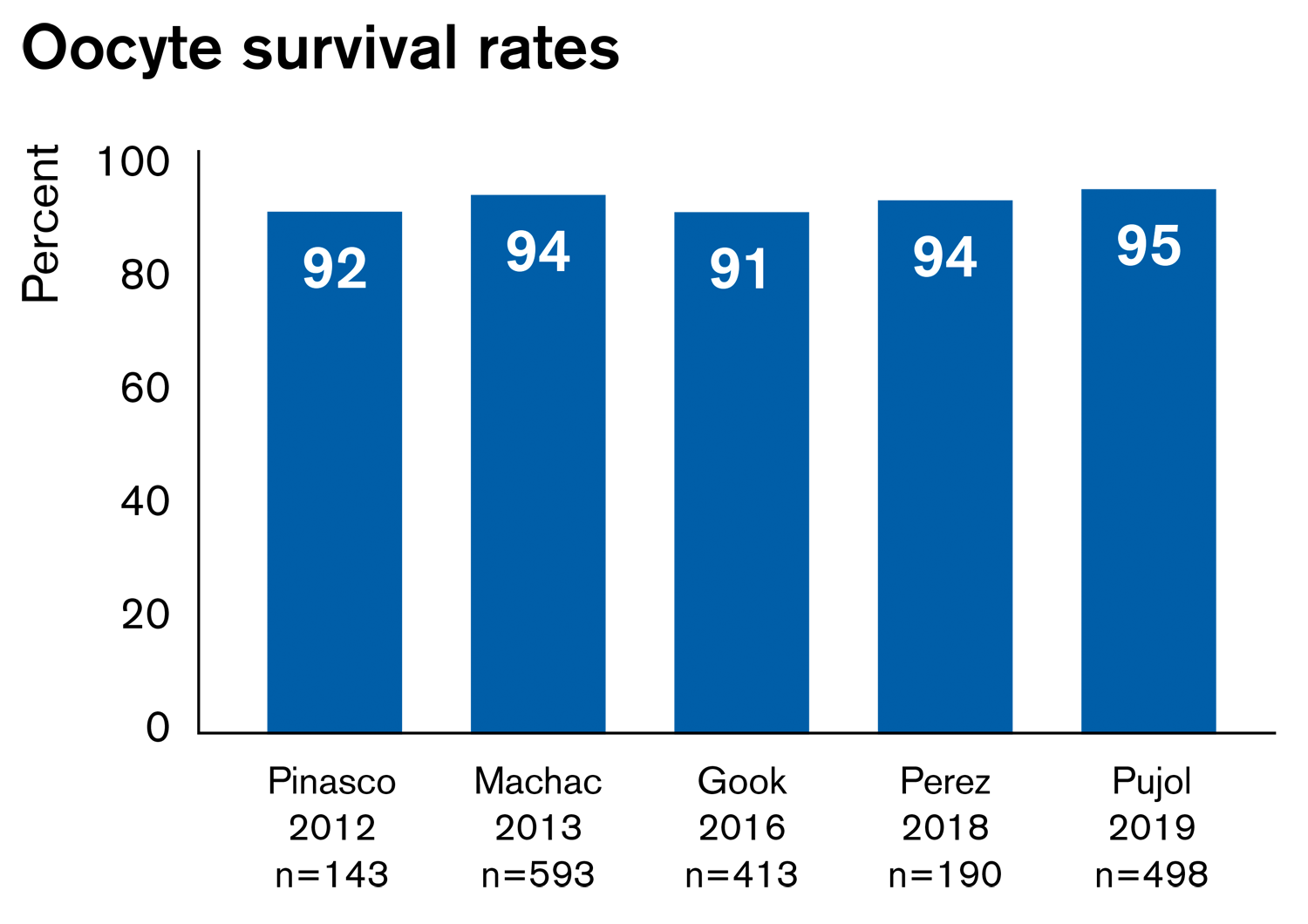
Results from multiple studies using the Rapid-i Kit show excellent survival and clinical pregnancy rates for both oocytes and blastocysts (figures below).
|
See all references below. |
|
Weighing up the pros and cons of closed and open systems
Vitrification is an important part of IVF treatment and modern technological advances ensure equally high survival rates using both closed and open devices. As only closed devices provide absolute biosafety for vitrified samples, we advocate that they are the best choice for vitrification of your patient’s oocytes and embryos.
- The closed Rapid-i Kit ensures a very high survival rate with 100% protection from possible contamination.
- Regulatory requirements in many countries are shifting towards the use of closed devices.
- The potential effects of SARS-CoV-2 virus on assisted reproduction outcomes are not evident yet, but the use of the Rapid-i Kit avoids possible risks.
References
- European Society of Human Reproduction and Embryology. ESHRE guidance on recommencing ART treatments. https://www.eshre.eu/-/media/sitecore-files/Guidelines/COVID19/ESHRE-Guidance-on-Recommencing-ART-treatments_update-04052020.pdf?la=en&hash=A584F8A306C570BE7648C167CB190F994E21F05A
- Adiga SK, Tholeti P, Uppangala S, Kalthur G, Gualtieri R, Talevi R. Fertility preservation during the COVID-19 pandemic: mitigating the viral contamination risk to reproductive cells in cryostorage. Reprod Biomed Online. 2020 Dec; 41(6): 991–997.
- Bernal DP, Chang C, Elliot TA, Elsner CW, Toledo AA, Nagy ZP. Clinical evaluation of the Cryolock device as a carrier for vitrification of blastocyst stage embryos obtained from cryopreserved donated oocytes. Fertil Steril. 2009; S92,3.
- Bielanski A, Nadin-Davis S, Sapp T, Lutze-Wallace C. Viral contamination of embryos cryopreserved in liquid nitrogen. Cryobiology. 2000 Mar;40(2):110-6.
- Bielanski A, Bergeron H, Lau PCK, Devenish J. Microbial contamination of embryos and semen during long term banking in liquid nitrogen. Cryobiology. 2003 Apr;46(2):146-52.
- Bielanski A, Vajta G. Risk of contamination of germplasm during cryopreservation and cryobanking in IVF units. Hum Reprod 2009;24: 2457–67.
- Criado E, Moalli F, Polentarutti N, Albani E, Morreale G, Menduni F, Levi-Setti PE. Experimental contamination assessment of a novel closed ultra-vitrification device. Fertil Steril. 2011 Apr;95(5):1777-9.
- De Munck N, Santos-Ribeiro S, Stoop D, Van de Velde H, Verheyen G. Open versus closed oocyte vitrification in an oocyte donation programme: a prospective randomized sibling oocyte study. Hum Reprod. 2016 Feb;31(2):377-84.
- Desai N, Goldberg JM, Austin C, Falcone T. The new Rapid-i carrier is an effective system for human embryo vitrification at both the blastocyst and cleave stage. Reprod Biol Endocrinol. 2013 May 15; 11:41.
- Desai N, Ploskonka S, Goodman L, Attaran M, Goldberg JM, Austin C, Falcone T. Delayed blastulation, multinucleation, and expansion grade are independently associated with live-birth rates in frozen blastocyst transfer cycles. Fertil Steril. 2016 Nov;106(6):1370-1378
- Gook DA, Choo B, Bourne H, Lewis K, Edgar DH. Closed vitrification of human oocytes and blastocysts: outcomes from a series of clinical cases. J Assist Reprod Genet. 2016 Sep;33(9):1247-52.
- Gunst J. et al, Data on file, 2019. Slow developing embryos undergoing compaction or cavitation on day 5 substantially contribute to live birth rates after single day 6 vitrified-warmed blastocyst transfer, P-135, 36th annual meeting of the Society for Human Reproduction and Embryology, 2020.
- Hashimoto S, Amo A, Hama S, Ohsumi K, Nakaoka Y, Morimoto Y. A closed system supports the developmental competence of human embryos after vitrification : Closed vitrification of human embryos. J Assist Reprod Genet. 2013 Mar;30(3):371-6
- Iwahata H, Hashimoto S, Inoue M, Inoue T, Ito K, Nakaoka Y, Suzuki N, Morimoto Y. Neonatal outcomes after the implantation of human embryos vitrified using a closed-system device. J Assist Reprod Genet. 2015 Apr; 32(4): 521–526.
- Katayama KP, Stehlik J, Kuwayama M, Kato O, Stehlik E. High survival rate of vitrified human oocytes results in clinical pregnancy. Fertil Steril. 2003 Jul;80(1):223-4.
- Lane M, Schoolcraft WB, Gardner DK. Vitrification of mouse and human blastocysts using a novel Cryoloop container-less technique. Fertil Steril. 1999 Dec;72(6):1073-8.
- Luyet BJ and Gehenio MP. Life and Death at Low Temperatures. 1940; 1st ed. Normandy, MI: Biodynamica; 1–328.
- Luyet BJ. The vitrification of organic colloids and of protoplasm. Biodynamica. 1937; 1:1–14.
- Machac S, Hubinka V, Larman M, Koudelka M. A novel method for human oocyte vitrification with a closed device using super-cooled air, Fertility and Sterility. 2013;100 (3), S108. 6.
- Machac S, Hubinka V, Larman M, Koudelka M. A novel method for human oocyte vitrification with a closed device using super-cooled air. Fertil Steril. 2013 Oct;100(3):S108.
- Perez O, Tilley B, Navarrete G, Lay L, Little LM, Gada R, Chantilis S, Show l. Oocyte vitrification using a new vitrification medium and a new closed vitrification device. A sibling oocyte study, Fertility and Sterility. 2018;110, Issue 4, e179 -e180. 7.
- Pinasco M, Hickman T, Russell H, Rashiv B. Oocyte Vitrification Freeze/Thaw Survival Rates Using an Open versus a Closed System, Fertility and Sterility. 2012;97 (3), S18, P-27. 5.
- Pujol A, Zamora MJ, Obradors A, Garcia D, Rodriguez A, Vassena R. Comparison of two different oocyte vitrification methods: a prospective, paired study on the same genetic background and stimulation protocol. Hum Reprod. 2019 Jun 4;34(6):989-997.
- Scorio R, K Thong J, Pickering SJ.Single blastocyst transfer (SET) and pregnancy outcome of day 5 and day 6 human blastocysts vitrified using a closed device. Cryobiology. 2018 Oct; 84:40-45.
- Sciorio R, Thong KJ, Pickering SJ. Increased pregnancy outcome after day 5 versus day 6 transfers of human vitrified-warmed blastocysts. Zygote. 2019 Oct;27(5):279-284.
- Seki S and Mazur P. The dominance of warming rate over cooling rate in survival of mouse oocytes subjected to a vitrification procedure. Cryobiology. 2009 Aug;59(1):75-82.
- Tedder RS, Zuckerman MA, Goldstone AH, Hawkins AE, Fielding A, Briggs EM, Irwin D, Blair S, Gorman AM, Patterson KG, Hawkins AE, Gormon AM, Heptonstall J. Hepatitis B transmission from contaminated cryopreservation tank. Lancet. 1995 Jul 15;346(8968):137-40.
- Vajta G, Holm P, Kuwayama M, Booth PJ, Jacobsen H, Greve T, Callesen H. Open Pulled Straw (OPS) vitrification: a new way to reduce cryoinjuries of bovine ova and embryos. Mol Reprod Dev. 1998 Sep;51(1):53-8.
- Vajta G, Rienzi L, Ubaldi FM. Open versus closed systems for vitrification of human oocytes and embryos. Reprod Biomed Online. 2015 Apr;30(4):325-33.
Topics: Vitrification, IVF community insights, Managing your IVF clinic, cryostorage, Reproductive Care